Wendy Myres, MAT, CCC-A, reflects on her 37 years of cochlear implant experience to discuss the evolution of CI technology and the hearing industry as a whole.

Cochlear: What do you remember from when you first started working with CIs?
Wendy Myres: I started working with cochlear implants (CIs) in 1983. Back then our patients had bilateral profound sensorineural hearing loss. Hearing aids were usually large body-worn aids or large analog behind-the-ear (BTE) devices. CIs consisted of one-ball electrode and we used an oscilloscope and an interface box to set the device with a screwdriver. We would establish the threshold level or carrier signal using stimulation from the interface box and then make a sound like “oooo” and watch the oscilloscope to set the maximum comfort level.
Early CI sound processors
The first CI sound processors I worked with were metal boxes that took two 9-volt batteries. The patient had to unscrew the box to open it and change batteries. Initially we did not have the use of magnetic coupling between the internal and external transmitter, so we would either place a bracket on the patient’s eyeglass temple or they could wear a wire headband to try to keep the coil in place. The microphone was glued to a wire hook we placed over and behind their ear or glued to the eyeglass temple. That’s why I have to laugh when my patients today look at the size of the Nucleus® 7 Sound Processor or Kanso® 2 Sound Processor and ask if there is anything smaller.
Evolution of indications and outcomes
Another big difference was the fact that we initially started clinical trials with children no younger than four years of age – we’ve learned a lot since then. If a hearing aid was of no benefit, we would fit them with a loaner vibrotactile device so that we could work with them on the basic suprasegmental features they would be hearing with the single-channel CI. Although we had a few pediatric single-channel patients who achieved open-set speech understanding, most of the patients just experienced sound awareness and lipreading enhancement with their single-channel CIs. Expected outcomes have changed so much because most of the adult patients were going from nothing to something, they were so appreciative to have sound awareness and feel more involved in what was going on around them. The sound can help their lipreading scores improve. Today our appointments are usually two-hours in length. Back then we would see them for almost a whole week of “Basic Guidance”. They would come for four hours for four days in a row and received intensive auditory training while they learned to listen with their CI.
Cochlear: What indication changes do you consider to be most pivotal in the CI industry?
Wendy Myres: I would say the most pivotal change is implantation of individuals with residual hearing. I’m not referring to those who qualify for Hybrid implants necessarily, but those who used to be considered “borderline” candidates, at best. It can be heart-breaking to turn someone away because they scored too well on our pre-op candidacy test protocol, but you know they are obviously struggling in their day to day communication. Early on, I never thought we would implant someone who is able to use the telephone, but when they are in a group setting or other noise, they have trouble understanding and the implant makes their lives easier.
Cochlear: How have outcomes changed with regard to these changes?
Wendy Myres: Patients now expect to understand speech without visual cues. This is not always possible for everyone and can be frustrating for those who don’t achieve that, but in the majority of cases we now see patients understanding speech without visual cues in normal quiet environments when they use their CIs consistently. It has also been rewarding to watch the young children who were implanted as infants and toddlers now using normal speech and language and functioning well in their chosen line of work. Those kids, who at one time used to hide under a table or refuse to play whatever listening game was offered, now come back and share all the good memories they have of their time coming to the clinic as young children.
Cochlear: How did you counsel your patients about making phone calls 30 years ago? How do you counsel them about phone calls now?
Wendy Myres: Back then, when a patient didn’t have speech understanding, we would train them to use a Telephone Code. The patient had to take control of the conversation, explaining they were deaf, but could communicate with the caller by asking questions. The caller was then instructed to respond by saying either “No”, “Yes” or “I don’t know that”. It was cumbersome and difficult for many who were embarrassed and didn’t want to tell others what to do. Now of course, we have wireless streaming and/or speaker phones, or captioning even on our cell phones and don’t routinely teach them Telephone Code.
Cochlear: What evolutions in the Cochlear™ Nucleus® system offering have you found most significant to you and your patients?
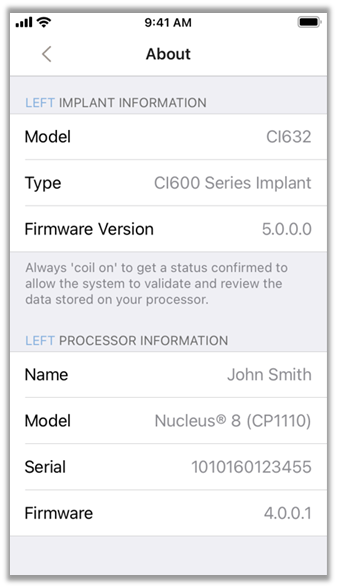
Wendy Myres: It’s great to be able to monitor the patient’s electrode impedances. Having the magnetic coupling of the internal and external transmitter is also helpful of course, and now that we have the MRI compatible implants, it has made a big difference for our patients who would otherwise have to have the magnet removed and use the retainer disk. However, I think the wireless connectivity has been the most exciting and significant change, especially for the patients.
Cochlear: Would you highlight a story about your earliest implanted Cochlear Nucleus 22 patient?
Wendy Myres: The nicest thing about the early days when our caseload was not as big was that we really got to know our patients and their families very well. One young man I can think of was not our first N22 recipient, but at the time he was implanted in 1995 he was one of our youngest as he was under two years of age. He received an N22 in his right ear only and because he had excellent therapy and follow-up, attending all of his recommended appointments he did very well. In looking back at his chart, it would appear he also used most of Cochlear’s earliest sound processors as they developed with the exception of the WSP body-worn. The earliest record I could find was when he was using the ESPrit™ 22 3G, which we thought was a big deal as the first BTE processor. He is 27 years old now.
This case was always special to me because he was our first child implanted before age two. He did so well that when I was traveling with my family one year we ran into him with his parents at the airport. I introduced this patient to my husband who later told me that if I hadn’t told him he was deaf and had a CI he would have never known. I felt very proud of what we do with our CI patients in providing them with hearing and a chance to communicate more easily.
Current global environment and delivery care
Cochlear: How do you envision Remote Care being delivered to cochlear implant recipients?
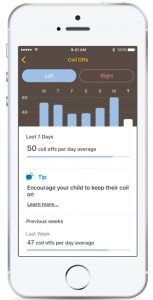
Wendy Myres: Although there are many implant centers across the country, we still have patients who come from out-of-state or at least three-to-four hours away. For our more elderly patients, travel can be difficult, as it can be for the parent of child who may have many other children to take care of. I always have thought that those who have grown up with CIs and are more tech-savvy may be able to somehow connect to a modem at home and check their telemetry, adjust their MAPs, etc. While this may not be for everyone, it would be helpful to many.
Cochlear: What are you looking forward to in the CI field?
Wendy Myres: Speaking for my patients, they would like even smaller processors. CIs have evolved so much in my 37 years that it has never become boring. As we improve patient care, we have been able to work more frequently with those with multiple medical issues, and I’m looking forward to potential future indication changes to be able to help even more patients.
To read more, subscribe to Cochlear ProNews.
About the author: Wendy Myres has worked at Riley Hospital for Children at IU Health working with the Cochlear Implant Program for over 37 years. Prior to that time, Wendy worked with hearing aids, provided audiology services in a ear, nose and throat private practice, worked providing therapy for hearing impaired students in the Indianapolis Public Schools, and provided diagnostic audiology services at Indiana University Health Methodist Hospital before coming to Riley Hospital for Children at IU Health. As a member of the Cochlear Implant Program, Wendy works with patients of all ages, from infants to senior citizens.
This reflects the views of Dr. Myres.
Cochlear Nucleus cochlear implants are intended for use on individuals 18 years and older who have bilateral, pre, peri or postliniguistic sensoirneural hearing impairment and obtain limited benefit from appropriate binuaral hearing aids. For complete indications, please refer to implant instructions for use.
The Hybrid L24 Implant is approved in the U.S. only for unilateral use in adults 18 and older. For complete indications please refer to instructions for use.