James Connor Sullivan, AuD, CCC-A, F-AAA, discusses his experience as an audiologist and recipient, as well as the future of the cochlear implant industry.
How did your experience as a recipient draw you to the field of audiology?
Dr. Sullivan: As a child, my family always raised their kids that they would have to go to college after graduating high school. As the only person with hearing loss in my family, I was treated no differently. I went through all of my grade school with bilateral hearing aids, and it wasn’t until college that I became a candidate for a cochlear implant.
Prior to getting a cochlear implant, I actually never wanted to be an audiologist. When I was in high school, I always thought I wanted to work in a theater program working behind the scenes as a lighting technician, so I enrolled into a selective theater program in Oklahoma. It was during my first semester of my undergraduate program that I had a pretty significant hearing fluctuation, making me a candidate for a cochlear implant.
As an avid researcher of everything technology, I turned to the web and anything else I could get my hands on to get any information I could about the cochlear implant process, trying to figure out “what a cochlear implant sounds like.” It very quickly became apparent to me that getting good, reliable and accurate information for young adults about cochlear implants is very difficult.
Most young adults with hearing loss are in an awkward stage of their life (for many reasons). Most young adults are trying to figure out their financial situations, career goals, health insurance coverage, how to pay for hearing technology as they are losing coverage, all in the midst of possibly transitioning out of their pediatric audiology clinic and into their adult audiology clinic with a new provider.
I was young, broke, unhappy with my major as a freshman, unable to afford healthcare or new hearing aids, and my hearing had a pretty significant shift in my hearing and word understanding. As part of the cochlear implant approval process I realized that I had a unique insight that most people rarely get to experience or share with their patients.
The day I got activated with my cochlear implant I changed my major from theater to audiology because CI audiologists get to change our patients’ lives every day. I always knew I wanted to do something that had a true impact in others lives and little did I know how much I’d love getting to do it.
How has the current global environment changed the way you deliver care?
Dr. Sullivan: COVID-19 has thrown a wrench in 2020. I think that the pandemic has made providers think about each procedure and process, and ensure that what we are doing is beneficial to the patient and to the office as a whole. As part of this review, I believe that we have found some things to increase the efficiency of our clinic to help make a lasting change in the patient experience.
- Prior to COVID-19, our clinic utilized primarily paper case histories. We have now moved to all digital, allowing for appropriate triaging of patient appointments and for our clinical assistants to move up appointments as medically indicated.
- As face masks are required in all clinical spaces, we have expanded the use of voice-to-text software throughout our iPads® for our patients with significant hearing loss or language barriers.
- We have added virtual appointments for any and all appointments that have the ability to be conducted virtually, including device selections and counseling appointments.
How do you empower patients to achieve hearing goals and outcomes?
Dr. Sullivan: We have all of our cochlear implant patients establish care with an auditory verbal therapist to assess their needs and set appropriate goals. From an audiology standpoint, it is important to educate the patient, but not over-educate them on all of the intricacies of their equipment. It is VERY easy to get overwhelmed the first day.
At my activation appointments, I tell the patients that they need to “focus” on three things during their first few days with the device, adding more layers of complexities as I see the patient for their follow-ups.
1. How to change the battery and put the device on.
2. Focused listening therapy, at least 20-30 minutes a day.
My go-to apps are AngelSounds™ and Bring Back the Beat. Later I encourage audiobooks.
3. Progressing through the progressive MAPs.
I typically set a schedule for when to progress, every two days progress to the next MAP. By the next time I see them they’ll be on the appropriate MAP.
At the end of the day wear time and auditory stimulation is the name of the game. As the patient comes for their follow-ups and they display that they have an appropriate grasp of the first concept, then I’ll add in information like accessories.
Is hearing therapy involved?
Dr. Sullivan: In order to ensure the patient has appropriate access to sound, we always check Ling Sounds during their MAPping to ensure an appropriate MAP has been completed. Once appropriate access to all the Ling Sounds has been established, the patient needs to establish care with hearing therapy.
Hearing therapy is an integral part of our cochlear implant team. As previously mentioned, we have established our patients with our auditory verbal therapist in the area. We also encourage at-home exercises and show them in the clinic to ensure understanding of the tools.
How are outcomes and quality-of-life measured?
Dr. Sullivan: We measure outcomes through the SSQ, the Tinnitus Handicap Inventory (if they have Tinnitus) and the Nijmegen Cochlear Implant Questionnaire. These are administered through an online survey site on an iPad. In addition, we regularly assess our patient’s performance through functional testing with CNC and AzBio (in quiet and in noise as appropriate) testing.
Can you touch on awareness/access to care in the cochlear implant industry?
Dr. Sullivan: It’s no secret that cochlear implants are significantly underutilized by patients who could benefit from them. I think that the 60/60 guideline (Zwolan et al. 2020)1 should really be in every clinician’s mind when conducting any audiological examination.
If a patient has less than or equal to 60% word recognition in either ear, or if their pure tone average is at or less than 60 dB HL for either ear, a clinician should refer the patient for a cochlear implant evaluation. It is important to stress that just because you get evaluated for a cochlear implant, it does not mean you are receiving a cochlear implant. I always look at these appointments as information gathering sessions.
Per Zwolan et al. 2020, if utilized as a screening guideline this screening has a 96% detection rate and a 34% false positive rate.
It is important to educate fellow clinicians, providers in the area and patients about the ever-changing cochlear implant landscape.
What excites you the most moving forward in the CI industry?
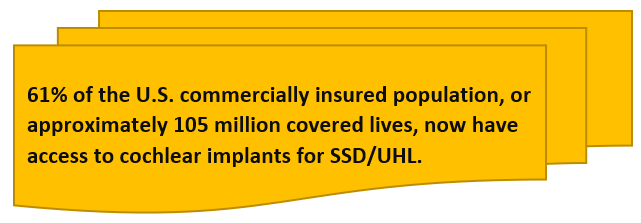
Dr. Sullivan: I’m most excited about the expanded access to this life-changing technology. As previously mentioned, I never would have even considered being an audiologist and now I get to work with cochlear implant patients every day. I’m looking forward to the evolution of cochlear implant processor technology and providing access to patients who otherwise would have never received access to this technology.
For more helpful resources, subscribe to the Cochlear ProNews.
About the author: Dr. Sullivan is an audiologist who works in the Houston area with patients who have hearing loss. Dr. Sullivan, also born with a hearing loss, enjoys using both his personal and professional experiences with his cochlear implant and hearing aid to aid in the treatment of his patients. Dr. Sullivan has presented both nationally and internationally on several topics, including Large Vestibular Aqueduct Syndrome, the disorder that resulted in his hearing loss. He is passionate about using his personal experiences alongside clinical knowledge in audiology to help patients across the lifespan and their families who are impacted by hearing loss.
References:
- Zwolan, Teresa A.; Schvartz-Leyzac, Kara C.; Pleasant, Terrence Development of a 60/60 Guideline for Referring Adults for a Traditional Cochlear Implant Candidacy Evaluation, Otology & Neurotology: April 20, 2020 – Volume Publish Ahead of Print – Issue – doi: 10.1097/MAO.0000000000002664
©2020. Apple, the Apple logo, FaceTime, Made for iPad logo, Made for iPhone logo, Made for iPod logo, iPhone, iPad Pro, iPad Air, iPad mini, iPad and iPod touch are trademarks of Apple Inc., registered in the U.S. and other countries. App Store is a service mark of Apple Inc., registered in the U.S. and other countries.