Cochlear Americas understands the importance of assisting patients and providers with payer advocacy and navigating the health insurance landscape. We have dedicated experts staffed to support reimbursement and policy. We are here to help. Below, our Health Economics and Reimbursement team provide answers to commonly asked questions regarding our patient insurance support program for both new patients seeking to be implanted as well as recipients wanting to upgrade their sound processor.
What is Otologic Management Services and how can this program help patients?
For new patients seeking to be implanted, Otologic Management Services, Inc. (OMS), a division of Cochlear Americas, is a dedicated team of reimbursement specialists who are available to help medically qualified patients obtain the necessary insurance approval and assistance in appealing denied coverage for Cochlear’s Systems.
OMS is available at no cost to eligible patients without regard to their provider’s business relationship with Cochlear. OMS provides its services to patients seeks input from patients’ healthcare providers during the process.
How does OMS support patient access to Cochlear’s hearing implants?
OMS helps obtain approvals for the initial implant system by addressing coverage issues and can appeal to the state’s Department of Insurance (when applicable). Each team member has experience working with large and small health plans and has the knowledge to navigate health insurance policies. OMS is extremely knowledgeable when it comes to Cochlear’s products and has vast experience working with payors on approval and appealing denials.
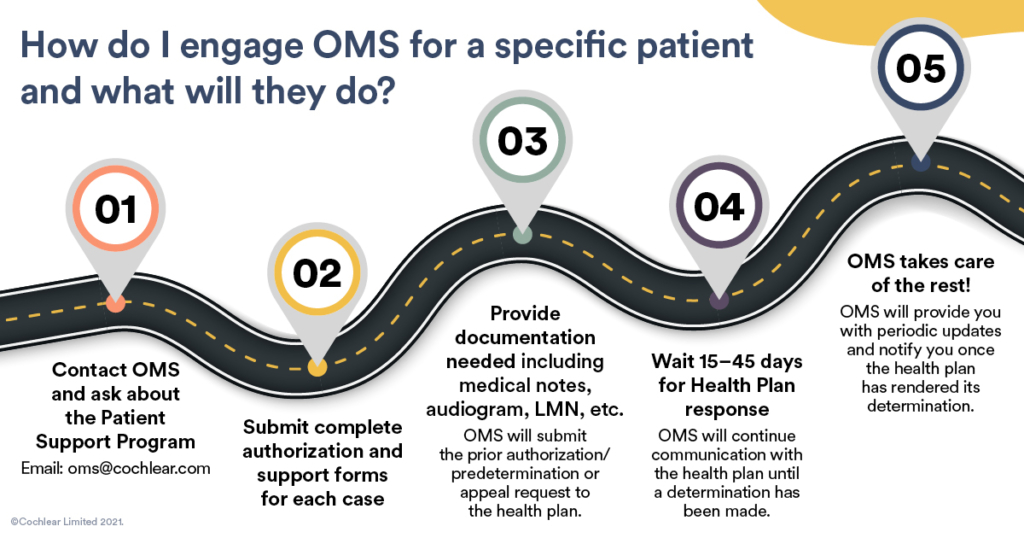
For new patients seeking to be implanted, their provider must complete a few steps:
- Patient insurance support program overview (only required for center’s first submission)
- Patient information form
- Patient release of information form
- Patient authorization to provide services form and applicable medical records, insurance card, etc.
A preauthorization or predetermination request typically takes 15-45 days for a response from a Health Plan and appeals can take longer. OMS follows up with the health plan every 10 days and notifies all parties once a determination is made.
To see additional information on OMS Pre-Surgical Support and OMS Claim Submission process watch one of our webinars: https://www.cochlear.us/ProfessionalWebinars. You can contact OMS by email at OMS@Cochlear.com or by phone at 800-633-4667 (option 4).
What does coverage look like for Medicare, Medicaid, and private insurance patients for hearing implants?
Medicare has established policies on cochlear implants and osseo-integrated bone anchored systems. It is critical that clinical documentation supports medical necessity requirements. Traditional Medicare pays 80% of the Medicare approved amount (different from charges) and patients are usually responsible to pay a deductible and 20% coinsurance under Part B benefits, unless they have a Medicare Supplement Insurance Plan or a Commercial Secondary Health Insurance Plan. Medicare Advantage plans are required to cover all Medicare approved services but may require prior authorization. Coinsurance, co-pays and deductibles will vary among Medicare Advantage plans.
Under the Early and Periodic Screening, Diagnosis and Treatment (EPSDT) federal benefit, state Medicaid programs are required to provide hearing services to Medicaid beneficiaries under the age of 21. Therefore, Cochlear Implants & Bone Anchored services are covered by state Medicaid programs throughout the US. Coverage and prior authorization requirements vary by state. Coverage for adult Medicaid recipients varies according to state specific guidelines.
For private or commerical insurance like Humana, Aetna or UnitedHealthcare each plan has their own medical policies and prior authorization requirements. Most commercial plans cover cochlear implants and osseo-integrated bone anchored systems. However, some plans may classify osseo-integrated bone anchored systems under the patient’s hearing aid benefits. Every patient has their own unique benefit package which outlines their coinsurance, deductibles, and out of pocket maximums based on the plan’s benefit coverage.
Cochlear has put together a Quick Tips for Obtaining Insurance Coverage to offer some best practices providers can implement to help maneuver through the insurance process. You can provide your patients with the following brochures to help answer questions on coverage:
Implantable hearing solutions – step-by-step guide to the insurance process
What are health plan requirements for seeking approval for a patient?
Most health plans require providers to:
- Seek advanced approval for all elective inpatient medical and surgical admissions, and most outpatient surgeries. Cochlear systems are typically outpatient procedures.
- Verify coverage and benefits of the patient’s treatment plan
- Provide applicable coding and medical necessity documentation for services/procedures requested
It’s important to know that just because an insurance plan finds a service medically necessary does not mean the patient has benefit coverage to pay for that service. Prior authorization and predetermination of benefits help avoid misunderstandings about financial liability.
What are predetermination and prior authorization best practices?
Be sure when scheduling surgery to allocate enough time to allow for a response from the Health Plan, which can take an average of 30 days. End of year response times from Health Plans may be delayed. Keep this in mind when scheduling patients and setting expectations for patients trying to optimize benefits by the end of the calendar year.
It is critical to verify coverage of a benefit. If reviewed separately from prior authorization, submit predetermination first to verify eligibility for benefits prior to submitting the prior authorization request. Submit both surgery and device codes and verify procedural requirements with the Health Plan. Many plans have the ability to submit online if you are submitting them on your own.
What services does Cochlear provide for patients once they have been implanted and need replacement parts or processors?
Whether your patient prefers to self-pay for their new sound processor or utilize their insurance benefits, our specialists can help your patients get their order started and navigate their insurance. Your patients can use Cochlear’s Reimbursement and Insurance Services and here are the steps that they can expect to take:
- Complete the necessary paperwork.
- Cochlear will request a Letter of Medical Necessity (LMN) from their clinician. This serves as a prescription and justifies a new sound processor is medically necessary for their hearing implant to continuously function. Keep in mind, health plans have their own definitions of what is considered medically necessary, but it typically includes anything that improves their hearing, or is required for the hearing implant to function.
- Cochlear’s Reimbursement and Insurance Services team will work directly with their health plan to collect all the necessary documentation to file the claim.
- Once we receive authorization from their insurance, we will collect any co-insurance due and ship their sound processor. They can expect it to arrive in 1-3 business days after shipping.
Your patients can visit our Insurance Support Center for more detailed information, links to the necessary forms and helpful videos. Generally, the sound processor upgrade process takes 6-8 weeks to process and ship when utilizing insurance benefits. You can provide this link to your patients that have questions about the upgrade process.
For more information and resources on how you can help your patients, visit our insurance and reimbursement website or to learn more about Cochlear services, download our Services report.
The information provided in this document is provided as guidelines only to address the unique nature of implantable hearing solutions technology. This information does not constitute reimbursement or legal advice. Cochlear Americas makes no representation or warranty regarding this information or its completeness, accuracy, fitness for any purpose, timeliness, or that following these guidelines will result in any form of coverage or reimbursement from any insurance company or federal healthcare program payer. The information presented herein is subject to change at any time. This information cannot and does not contemplate all situations that a health care professional may encounter. To be sure that you have the most current and applicable information available for your unique circumstances, please consult your own experts and seek your own legal advice regarding your reimbursement and coding needs and the proper implementation of these guidelines. All products should be used according to their labeling. In all cases, services billed must be medically necessary, actually performed, and appropriately documented in the medical record.