Cochlear Case Studies is a new series on Cochlear ProNews that highlights relevant clinical and surgical scenarios surrounding the latest hearing industry topics and research. We’re excited to partner with professionals to highlight their experiences surrounding specific patients. This first installment features surgeons, their cases and contributing factors for use of different electrodes.
Case Study
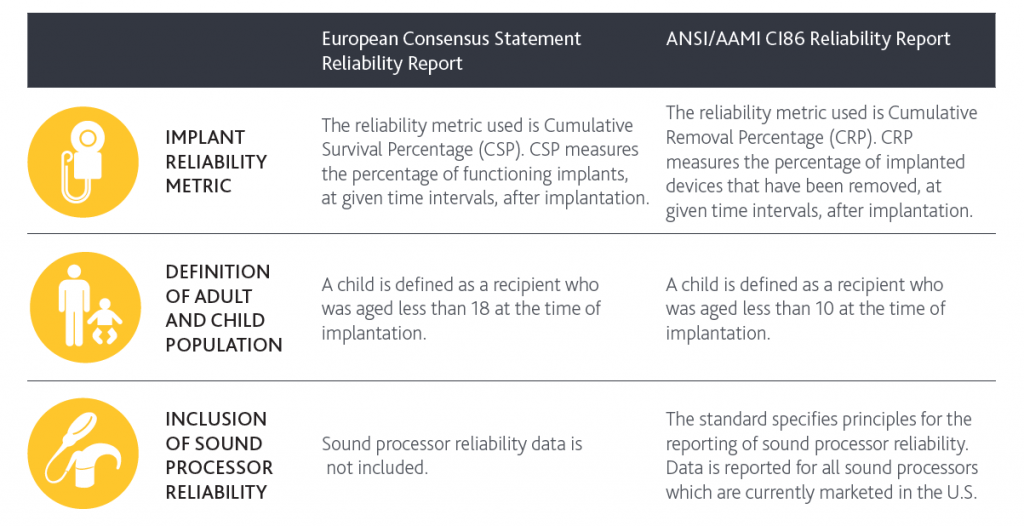
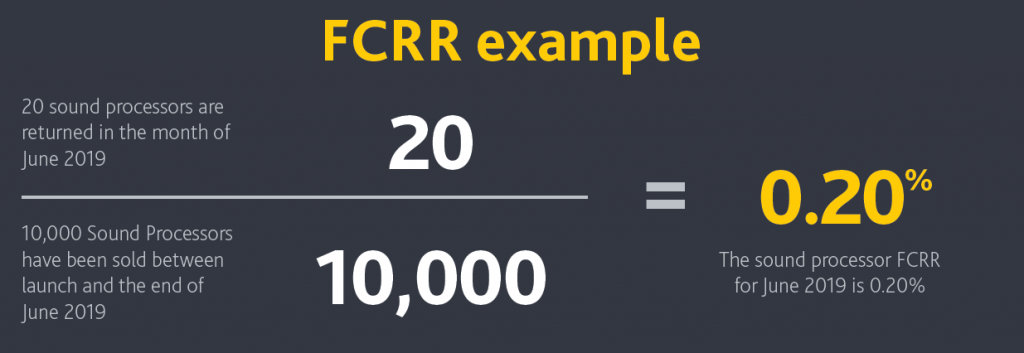
A 52 year old male sustained direct head trauma after falling down a flight of stairs. Immediately after the fall he reported no hearing bilaterally and the left side of his face was paralyzed. He was ultimately transferred to our medical center with a diagnosis of bilateral otic capsule violating fractures with the left side complicated by complete facial paralysis and a dural sinus thrombosis (CT images shown, MRV shown). Audiometry obtained five days after the fall demonstrated bilateral profound sensorineural hearing loss.
On day six after the fall, the patient was taken to the operating room for a left total facial nerve decompression via a translabyrinthine approach. A complete transection of both the 7th and 8th cranial nerves was identified in the fundus of the IAC, thus precluding placement of a cochlear implant in the left ear. He was brought back to the operating room approximately two weeks later (three weeks from the injury) to attempt placement of a right cochlear implant via a transmastoid approach.
The cochlea was visualized through the facial recess. A formal cochleostomy was created anterior inferior to the round window membrane as the fracture did involve the bony niche overhang. The scala tympani did appear to have some inflammation and granulation tissue; therefore, the depth gauge was inserted into the cochlear duct without removal of the stylet. Placement in the cochlear duct was confirmed with intraoperative X-ray. Once the depth gauge was confirmed in the duct and not in either the IAC or the fracture line, the depth gauge was removed and the CI632 Slim Modiolar Electrode was introduced into the cochlea.
I chose the CI632 for its perimodiolar position, MRI compatibility and slim profile to help minimize trauma in this already traumatized cochlea. Placement in the perimodiolar position was confirmed with X-ray intraoperatively. Electrical testing of the device was then performed (see tracings). The patient did have robust response of the cochlear nerve to NRT on several electrodes but had no response on others. Activation occurred four weeks postoperatively. He had responses in the low to mid frequencies and was able to detect sound and static with speech sounds. The patient has had his second stimulation is reporting improved detection and a recognition of speech vs noise!
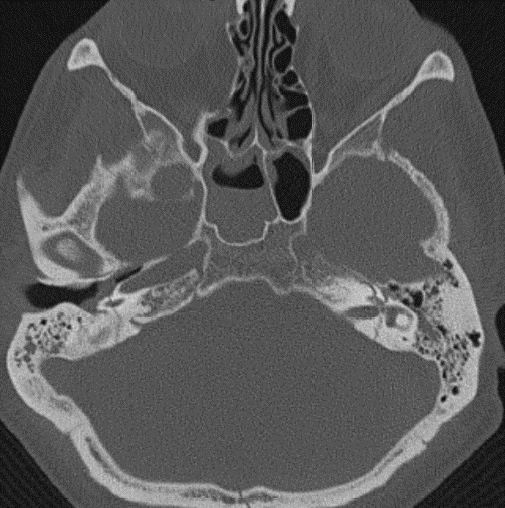
Image 1. Bilateral otic capsule violating temporal bone fractures. The left fracture transected the entire 7/8th nerve complex in the fundus of the IAC precluding implantation of the left ear. The right fracture spared the IAC and the facial nerve but resulted in pneumolabryinth and profound hearing loss.
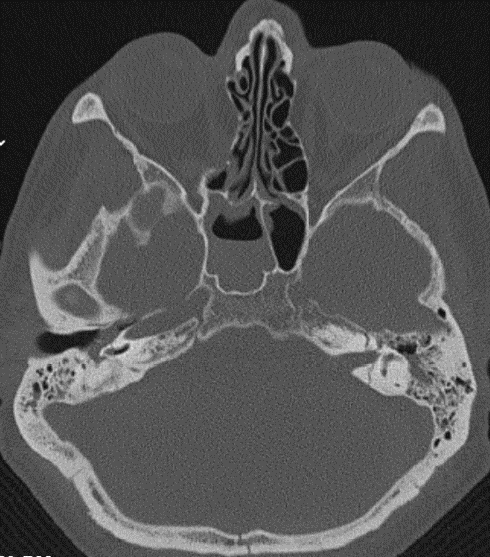
Image 2. Air in the right cochlear duct.

Image 3. MRV demonstrating decreased flow in the left transverse and sigmoid sinuses.
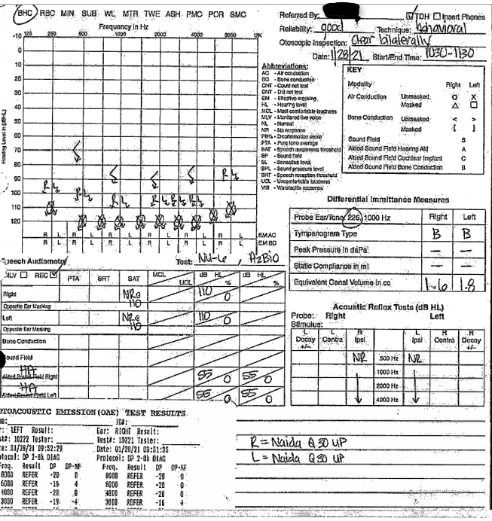
Image 4. Audiogram from five days after the injury demonstrating profound bilateral SNHL.
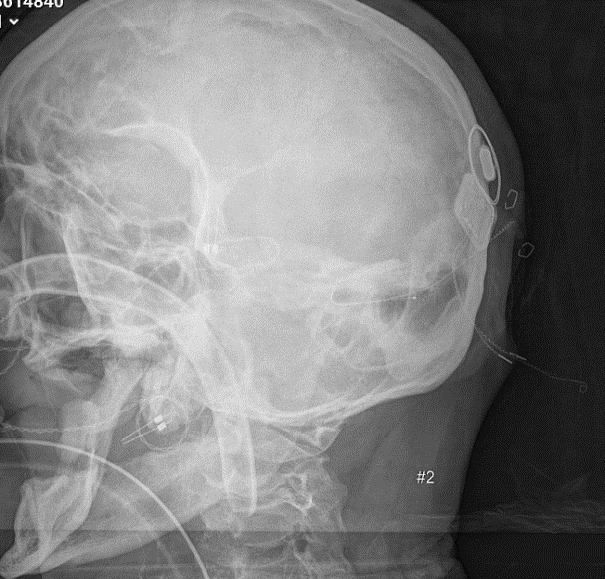
Image 5. Depth gauge in the cochlear duct. The gauge was inserted with the stylet in.

Image 6. Intraoperative skull X-ray demonstrating appropriate coiling of a CI632 electrode into the cochlear duct.
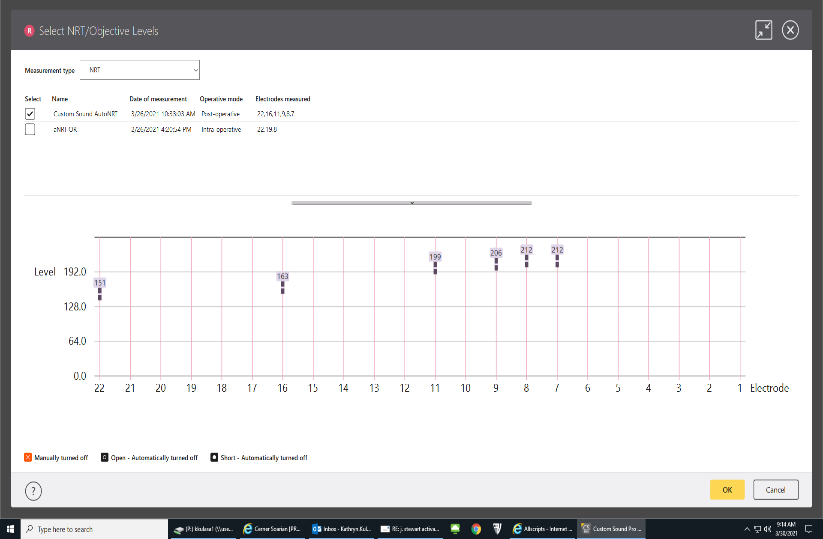
Image 7. Screenshot of a NRT obtained on the day of activation demonstrating variable responsiveness across the electrode array. This may represent injury to the cochlear nerve from shearing forces sustained at the time of fracture.
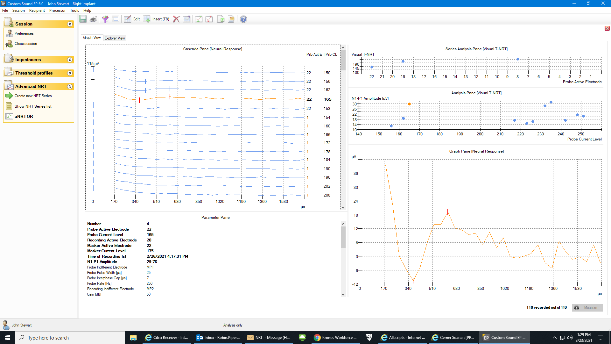
Image 8. Example of NRT from electrode 22.
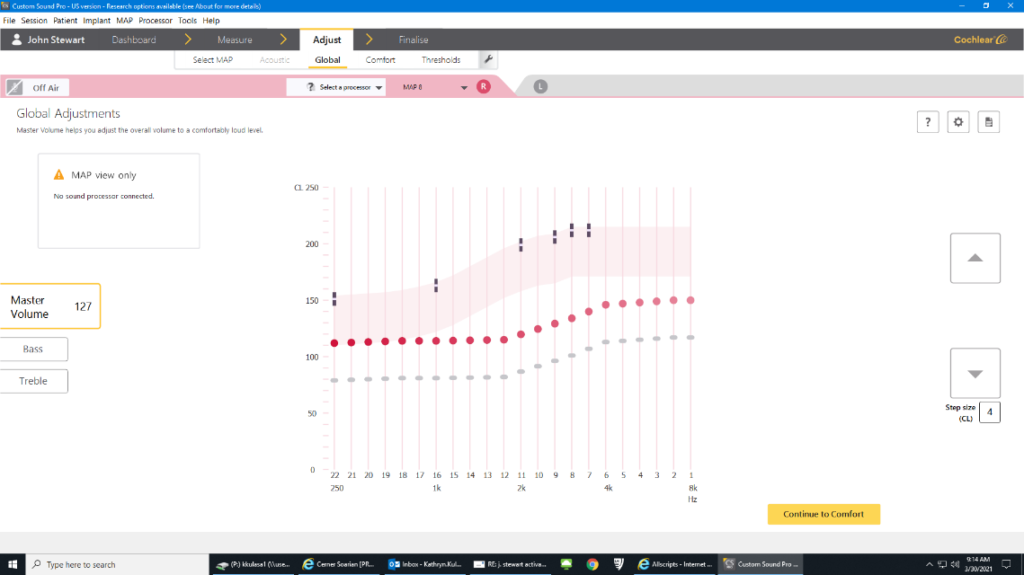
Image 9. Screenshot of his progressive map at the end of programing. His pulse width was widened to 37 from 25.
Are you a surgeon who has a case study to share? Contact mcoon@cochlear.com for a chance to be featured on Cochlear ProNews.

About the author: Dr. Mowry is an board certified otology/neurotologist who strives to provide excellent clinical care to patients while promoting the education of the next generation of leaders in the field. She treats both pediatric and adult patients who have dis orders of hearing, balance and the lateral skull base. Her interest in cochlear implants as a young medical student has translated in to a career of service to those with hearing disorders. She is also the residency program director for the University Hospitals Cleveland/Case Western Reserve University Otolaryngology department. She enjoys spending time with family, traveling, cooking and exercising.